Robotic Instrumentation - a deep dive (Exclusive Content)
- Steve Bell

- Jan 10, 2024
- 18 min read
Updated: Jul 30, 2025
In this EXCLUSIVE CONTENT post I've covered a deep dive into current and future robotic instrumentation. An analysis of current pros and cons - and future direction of simple and advanced instruments.
Intro to Robotic Instrumentation
People generally buy robots for two main features. 1) They want stable 3D vision and 2) They want wristed instruments (especially for suturing). There are many way that you can get to "wristed" instruments. With some being true wristed, and some being articulated and others being steerable or flexible.
All of these methods are aiming to give you three key spacial movements... Pitch, Yaw and roll. Which allows you to get the tip of the instrument in any location in the X Y Z planes.

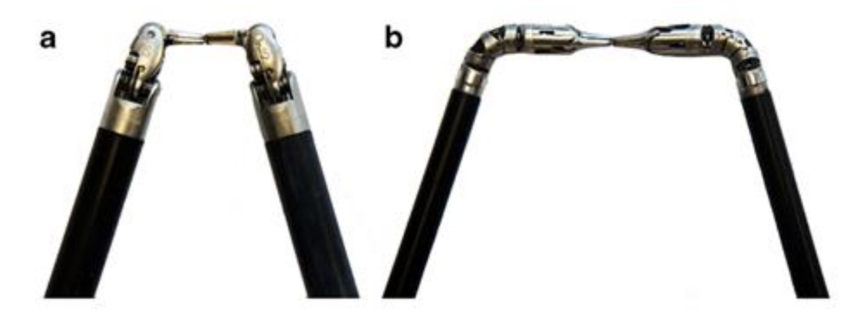
But not all "wrists" are equal. The gold standard wristed instruments rely upon a pitch joint, a yaw joint and a shaft roll mechanism. These are most frequently cable driven, where the cables work independently across pulleys to control the pitch and yaw, plus the opening and closing of the jaws.

As stated - the current gold standard in this design is the daVinci instrument range of 8mm instruments. There are a set of interfaces at the end of the instrument that connects to the drive pack of the robot arm. These rotation wheels are what move their cables through the pulleys. The robot's software controls the rotation interfaces to give the desired movements (in a simple explanation). The beauty of this type of design is an almost instant movement of the instrument tip to copy the hand movements of the user, and get almost instantaneous movement that mimics the human hand.
There are also "articulated" instruments. These are not considered true wristed instruments as they often just pitch or yaw in one direction and then put the roll of the instrument just at the tip of the instrument - not along the shaft.

These instruments are often less complex, so can be made more easily into 5mm, and more often than not they use solid push or pull rods to articulate the the single joint. The upside is simplicity with only needing one drive rod for articulation, and a rotation for the tip. The solid drive rod is also easier to control than cables. But this comes at a price. The instrument does not map in the same way to mimic the movement of human hand. It uses a combination of articulation and roll to orientate the tip. It does not allow the super complex and fluid 3D movements needed to say - push a suture through. This can often lead to less effective mapping of movements, and in some manoeuvres it can lead to a slight delay as the robot has to do articulation and rotation to find the right angle. It is clear from user feedback that the fully wristed instruments are much more user friendly and feel more natural.
There are multiple other ways that wristed function is mimicked such as flexible or steerable instruments. They often have segmented joints and combinations of solid straight and flexible shafts. They often use the flex shaft to mimic an "elbow - wrist" combination - and then tip rotation. This is good as they can be small diameter - 5mm. Plus you can deliver them very close to each other and then spread them through the elbow. So useful in say single port surgery. As applied by the daVinci SP.


There are various versions and mechanisms of how to create this effect. But they do have some drawbacks. Again not being true "wristed" instruments they do not have the same fluidity and inherent mapping as the 8mm wristed instruments. And the more complex the flexing mechanism, often the weaker the instrument is. With rigid straight sticks being the strongest in movement and gripping - wristed losing some strength and grip force - and flexible losing yet more.
In my experience of robotic surgery - surgeons really do buy the robot for fully wristed instruments. It feels natural to them and I think makes the surgical manoeuvres way easier. Learning curve faster and it is (this is gonna sound weird) more pleasurable to use.
So why doesn't everyone just make wristed instruments?
There are many reasons that companies may or may not make wristed instruments. Firstly is IP (Patents.) There are several patents still not expired on wristed instruments so some of that is a barrier is at that level. Other reasons are - they are super difficult to make - make well - make that work - and make that don't break. You cannot underestimate how difficult and precise the engineering is to make these instruments and have them work with precision to the micron. Deliver consistent forces and movements over the life of the instrument. It is not easy to make a wristed instrument - especially if you need to do it and at the same time be dodging the patent landscape.
Another reason is cost. That level of complexity in an instrument makes it very expensive to make. The components are complex and expensive - and the manufacturing is difficult. For that reason it is very difficult - almost impossible (in my mind) to make a disposable instrument fully wristed at a cost that would be acceptable and at a quality that is still as high as the gold standard. The only real way these expensive instruments make sense is if they are used 10 or more times - to cover the high cost of purchase vs a disposable laparoscopic instrument.
Some companies have tried early on to have 5mm articulated style instruments - such as the Senhance range. But from what I have seen and heard - they were not received well. And I do believe that their new product LUNA will move to fully wristed instruments; as they've understood that the market really wants fully wristed instruments - full stop.
The entire argument of surgeons "wanting" articulated instruments on a robot will become interesting for Moon Surgical and Maestro. Not to go into too much detail now - but these are arms that hold lap straight stick instruments - in a semi robotic way. (Technically it's a SCARA system - but that's for another post and podcast.) It will be interesting if surgeons find the benefit of smart scope holding and 3rd instrument holding - compelling enough in certain procedures to outweigh the benefits of wristed instruments. I have my doubts but time will tell.
One final thing to consider about most current robotic instruments is the fact they are multiple use instruments - so need to be able to be cleaned and sterilised. That is no mean feat - and I will discuss that in depth in the next section.
Reusable vs disposable
Over the years there has been much debate about instrumentation being reusable or disposable. In laparoscopy the majority of instruments now are reusable - but some "critical" instruments have remained as disposables - such as the laparoscopic scissors. And these can be fully disposable or just the tips exchanged.
WHY? One of the issues with scissors is that they need to remain sharp - and as scissors get used - over time - the blades become dull. This is due to simple cutting actions on tissue - but more often than not it is a problem of electrosurgery. Especially monopolar electrosurgery (diathermy / Bovie) use.
As electric current runs through the instrument and across the scissors - if the electrosurgery is activated with the blades open, this can cause damage to the blades. And for this reason in heavy electrosurgery scissor procedures such as prostatectomy, scissors can be damaged quite easily. The final issue for scissors is there is a build up of burned tissue (eschar) and if this is rubbed off by the bedside team using abrasive sponges - then the blades can be damaged further.
Robotic instruments today are primarily multi use instruments with lives anywhere between 5 and 20 uses. As said earlier, the high complexity and precision of manufacturing means that the instruments for robots are very expensive to make. The economics of the instruments only becomes viable when the instruments are re-used multiple times.
But this becomes an issue. The last use of an instrument must be just as good as the first use. And at some point the cables start to stretch, the pulleys start to wear, the crimps start to strain, the electrosurgery wires that deliver the electricity start to fatigue, and also bio burden starts to build. Oh, and as stated before - the scissor blades start to get dull. It's just were and tear of thousands of articulations and movements - often with the instrument at the absolute limit of its engineering tolerances.
I've heard a lot of surgeons say "these things are just chipped to go off after ten uses because it's a scam. My lap instruments last for years." Well it's not true. The companies want the first use and last use to be as perfect as possible. And at a certain age - the instruments just wear out. Testing makes sure that the last use is as good as the first, and that is what caps the number of uses - to have lots of margin so that degradation of performance is not seen in the patients. Or worse... breakages. Yes it does work beyond the chipped life but there is no good data to say it is till good and safe.
There is one exception where the instrument usage may not get quite to the level of performance as the instrument gets older. Scissors. I've often seen scissors changed mid case as they are "blunt" - and it is hard for engineers to predict this as they just don't know what abuse the scissor has suffered in prior cases. Too much electrosurgery through open blades... cutting sutures with them (don't do that!!), cutting plastic drains, cutting catheters - I've seen it all. Scissors just take serious abuse.
Now let me return to the issue of bio burden and contamination. So these instruments are being used in a high pressure CO2 environment - where fluid and blood will be forced under pressure up the instruments, against gas seals, into very intricate and complex instruments with lots of nooks and crannies. Braided cables and electrosurgery cables. Lots of places for bio burden to get trapped. Then inside the shafts are complex cables and rods and irrigation tubes - all tubes within a tube. Complex and full of areas where any fluid that enters can get trapped.
So this means that the instruments are very complex to clean and then sterilise. It takes a very careful regime of cleaning, manoeuvring, flushing, ultrasonic washing and more to ensure that these complex instruments have as little bio burden as possible. And some bio burden always remains. Small amounts, but it is there. in all instruments. And as the level of acceptable bio burden becomes lower and lower - with Germany leading the charge - it is getting harder to make such complex instruments that can be cleaned and sterilised - and pass the new norms.
One answer to this is "make them disposable". In fact - Distal Motion with Dexter have created a range of fully disposable wristed instruments. With the intent to reduce that complexity of cleaning and sterilisation. Many have been staggered that a European country (the leaders of the greens) company has done this. But it could make sense. If the functionality of the instruments is as good as Intuitive -- (I've had mixed reports) --then this could be an interesting approach for clinics and ASCs that will struggle with instrument turn around.

It will ruffle some green feathers about waste. And the economics of this approach needs to be proven out. But the total cost of "use" plus "Sterilisation" Plus "Disposal" costs - could actually add up. It will be interesting to see how well they are received, and if this economic (and potentially political green) issue works. This could be a major plus for them in places like ASCs. Economics will be number 1 - for sure.
I predict that as we move to lower acuity - lower cost procedures - in alternate setting such as ASCs - then the discussion of disposable vs reusable will come to the forefront.
5mm vs 8mm
I've discussed a little about the fact some instruments are 5mm and some are 8mm. The current gold standard today is the daVinci 8mm. And that is interesting because Intuitive did have 5mm instruments in the past... but have seemingly decided to abandon them. There have been over 10 million procedures done with 8mm instruments - and generally for adult surgery - no one is really complaining that they are too big.
Let me dig in a little about 8mm vs 5mm instruments and give some background. For minimal access surgery (I get bugged by minimally invasive as you can have small incisions but do some major invasive work) you want to have the holes in the patient as small as possible. Smaller holes cause less pain, less chance of port site herniation and less chance of infection that returns you to surgery. So in laparoscopy the gold standard is - 10/12mm ports for the camera at the umbilicus - and 5mm for the rest of the abdomen where possible. Clearly a 10/12mm extra if you need to pop say a stapler through. But generally it is considered a 5mm port is better.
But this is where it gets a little complex and grey. A 5mm port doesn't technically mean it has a 5mm internal diameter. It means a 5mm instrument will pass down it. 8mm means the 8mm (or less) diameter of instrument will fit down it. Well sort of. Some 5mm ports will allow a 7.9mm instrument down them... yep. In any case why do we care about "Diameters" of instruments inside tubes... when what you care about is the size of the hole left in the patient. Right?
So imagine I have an inside diameter of 5mm but an outside diameter (just to stress the point) of 25mm. Technically that is a 5mm port !!! Plastic ports to be as strong as metal ports need to have thicker walls. Balloon anchored ports need double thickness walls. So a 5mm plastic port could have an outer diameter bigger than an 8mm metal port ! Go get your measures out...
And also - the hole in the patient isn't just dependent on the port (cannula technically) it also depends on what type of whole you stick in the patient. So if as a surgeon I cut a 10mm hole in the skin and carry on down and cut muscle and fascia to that size - I have a 10mm hole (slit). If I put a 5mm port in that ... it's erm... stupid. Or if I use a pyramidal cutting trocar tip - I could (with an 8mm trocar) cut an 8mm Mercedes-Benz shape hole in the abdominal wall. However if I use a dilating tip 8mm port that separates and stretches tissue, I may only leave a 6mm slit in the patient. So sizing is very complex.
The reason I delved into this rabbit hole is because the instrument diameter is irrelevant unless you match it up with the port type (cannula outer diameter and trocar tip type). But instrument size becomes very very important for the strength - length and durability of the instrument. Intuitive has long - strong instruments that can last 20 uses because they have 8mm instruments - with carbon fibre shafts.
5mm instruments have a cross sectional area of 19.63mm2
8mm instruments have a cross sectional area of 50.27mm2
or 2.6x more cross sectional area to get stuff down.
Engineers really really care about this. Because inside that shaft needs to run all of the cables to do pitch and yaw - that's forwards and backwards (attached to rods inside the instrument) plus electrosurgery cables and flush / irrigation tubes and all the gasket seal to stop CO2 and fluid flow. Being 8mm also allows you to have bigger pitch and yaw wrists - and all the components (such as pulleys) can be bigger.And all of this means you can use bigger cables, stronger components and more durable components.
5mm instruments theoretically gets you smaller holes (you must use real 5mm metal ports) vs 8mm instruments (using real 8mm metal ports). But the trade off of, length, strength and durability - can be massive. Smaller cables risk cable breaks sooner in the life of the instrument. And that could be a potential economics changer. I see that Asensus is launching LUNA with "really" 5mm fully written instruments.
Here's my fears for that. The instruments might not last as long - and may not have adequate forces compared to an 8mm instrument. But they should offer the patient benefits of a 5mm trocar hole. So it will be very interesting to see if the rest of the industry continue the way of Intuitive and Medtronic, Distal Motion, Medicaroid etc - or smaller instruments will become the preferred choice. So far a lot of people seem happy with 8mm instruments and the post operative holes they leave behind.
Two other things about 8mm vs 5mm - a) If you have an 8mm scope and stapler (near impossible in 5mm) then with 8mm you can hop between arms and ports. With a 10mm scope and 5mm instruments - you have some restrictions. b) I come back to cleaning. The smaller the diameter the harder they are to clean and remove all of the bio burden. So it will be very interesting how in reality the battle between 5mm and 8mm will pan out. Maybe it will be a combination of both? When you need big n strong use an 8mm. When you want small n fine... a 5mm?
End effectors and multi function
Here I want to dig in a little into the final "tips" of the end effectors and talk about range of those instruments and functionality of the instruments. At the end of the day - one of the things that counts most is the instrument tissue interface. And as surgeons have known for decades - the right tool for the right job. You may get sick of hearing this, but the absolute market leader is Intuitive surgical (I would hope so after 20 years head start on everyone). They have a staggeringly good range of instruments for multiple specialties. And this is important.

One of the most important things for a surgical robot (competitors take heed) is that it is capable to do an full array of surgical procedures across "all" specialties. So not only does Intuitive have regulatory clearance across the widest range of procedures... they have the right tools to do those procedures well. For the vast majority of procedures you need: Graspers, monopolar scissors, Maryland bipolar forceps, needle holders, hooks... and well... that's about it. But if you want to explore all procedures, and do them well, you need a much wider range of specialist tools. And that is just the basic tools.
Beyond that you then have some specialist tools such as dual functional graspers, specific tip up instruments, various needle holders and some with built in suture cut. Then you get into clip appliers and specific graspers for specialty jobs like applying bulldog clips.
This is where there is a gulf between the market leader and any other company. Interestingly the one company that has the second largest range of instruments - seems to be SSI the Indian Mantra robot and Mudra instruments . Some of this is born from the fact the owner inventor is a cardiac surgeon; and bucking the trend of any other company is focusing in on robotic cardiac as a major part of their procedure offering. Some very interesting cardiac products - so worth a look.

So that leaves the other companies - which as of January 2024 - they actually have a very limited set of end effectors. Yes they can do a lot of the procedures - but they may force surgeons to make tactical choices - or use suboptimal techniques. Medtronic for example does not have a monopolar hook (at the time of writing) which for many is a glaring hole in their product line up. Others don't have a Tenaculum or heavy toothed forceps. That will make things like myomectomies incredibly challenging. Not impossible - but not optimal.
These gaps in the portfolio will need to be filled if institutions are to be able to do the full range of procedures with ease.
Next there is a difference in quality of the end effectors. I've held most in my hands, and I can just feel the quality gulf between the class leader Intuitive and some others. And this does actually get translated into surgical performance. You don't need to look at too many videos to see that needle holding, energy application and tissue manipulation is variable across the platforms. This is in part due to the robot arms - but it is also highly dependent on instrument quality and the quality, in particular, of the end effector tips. Design, geometry, machining (or moulding), finishing are all combined with the yaw / pitch joints and cables. It determines if jaws are aligned or misaligned. How well they open and close, and how the inner surfaces interface with tissues. These may sound like small deals - but they can mean the difference between minutes or more of operating time as tissue management and needle management is either made easier of more difficult by the end effectors.
In the end, the winning companies will have the right instruments for the right procedures at the the right quality - and of course... for the right price.
Advanced instruments
One of the big differentiators between the robots (I feel) is going to come down to the battle of the advanced instruments. Either multi functional instruments - or super specialist tools like advanced energy or staplers. I will do detailed blog posts on both and do a very deep dive into both with my thoughts for the future.
But here I want to scratch the surface of the three classes of instruments above:
For surgical staplers - this will be a must for the robots. People will often say "but the bedside assistant can fire the stapler." "It's a great training opportunity." And in many teaching institutions and settings that is valid. However the majority of surgery is often conducted where the junior bedside is not quite as qualified. Or there is not a second assistant - as the economics don't allow (ASCs). In some places there is a nurse or physician's assistant - but their operating rights don't allow them to position and fire staplers. And in other settings the surgeon just wants primary control of the placement and the firing of the stapler. So in many paces a robotically controlled stapler is a must.
And for the staplers - you will need to have the full range of lengths and cartridges - for thick, thin, vascular tissue etc. And the firing cycle will have to be smart - adapting to the tissue as you go through the firing stroke. Ensuring good even tissue compression - staple formation and transection.

It is utterly clear that Medtronic & JNJ will have robots that exclusively sport their class leading lap staplers. But when? Hugo and Ottava are not yet cleared in the USA- and when they do it will not be with stapling systems - that is obvious.
Other than that, all other manufacturers will need to either build their own stapler - or partner up. And neither path is easy. Staplers (and I've been selling them for 30 years) are about trust in the product. And if you are a new robotic company - bringing out your new robotic stapler - you will need to generate masses of data fast. But you cannot. because your installed base of robots is too small - and you will be in a horrible catch 22. You will not be able to get to the millions of firings - in fact the hundreds of thousands or even tens of thousands fast enough to build confidence. You just won't have the number of robots doing enough cases.
If you partner with a stapling company - that has its own challenges of integration. I cannot stress how hard it is to get your own stuff to work on a robot - let alone when you start integrating other companies' products. The technical - team - data - regulatory and financial challenges to make it work (both need to make decent margin) will just go through the roof.

Next I'll discuss a little on advanced energy. The current standard in the robotic space is Vessel sealer extend and Synchroseal by Intuitive. This is the current bar. However the bar in laparoscopic is Ligasure by Medtronic. If Medtronic can bring Ligasure to the HUGO they take a leap ahead of a lot for the other companies. The product itself (even though Gen I will be straight) will have a lot of fans. And one thought is that as long as your grasper is wristed - you can manipulate tissue into the straight jaws of the Ligasure. So for the early days it might work. But sooner or later - as Intuitive improves Synchroseal - the gold standard will be wristed advanced energy. And it will be interesting to see which companies can race to a wristed vessel sealer first - and have it fast with clean cuts and 7mm vessels. Come with less than that and be rejected.
The last part I'll discuss is advanced instruments such as multifunction devices. Already we have suture cut needle drivers. They allow the suture to be cut without the need for the intervention of scissors. More instruments will become multi function through design and engineering. Bipolar graspers are already excellent graspers in their own right - but they can also deliver bipolar electrosurgery. Others such as Synchroseal can be used a s sealer, a divider and a dissector as well as a grasper. It does the role of four instruments in one.
Then you have clip appliers which are really an advanced instrument as it is very hard to apply enough force through a wrist to get an absolvable clip to engage and lock.
Future possibilities
So this brings me to the final part. What will be next for robotic instrumentation?
Already the direction of travel is clear with multifunction instruments. The reduction of instrument exchanges is a much requested need. That will reduce both time and cost. So I imagine that we will start to see clever end effector designs that can do grasp - dissect - needle hold - maybe even cut in one device. Of course the challenge will be safety and not cutting when you should be grasping - but as the robots get smarter this will be manageable.
I foresee end effector becoming smarter and incorporating sensors. Either for haptics (see my other post on the future of robots) or for tissue sensing. Doppler for blood flow? Or sensors for biomarkers or agents to look for tumour cells and tumour margins.
I think we will see more instruments introduced to deal with high caseload and faster turnover - being disposable or having disposable end effectors. Maybe scissors with interchangeable tips? Maybe reusable drive pack interfaces that you can attach different disposable wristed shafts to, in order to reduce cost. Re-usable housing with disposable shafts and tips.
There are also lots of patents floating around with straight and flexible instruments integrated for "reach around" instruments. I have my doubts about the usefulness but maybe in attempting to get to trans oral or transanal with a multi-arm robot more efficiently there could be some utility.
I think massively extended lives will happen for some instruments when testing allows getting to 50 or 100 lives for low criticality instruments like graspers. This will help to shape the economics for places like ASCs where margins are way smaller.
As companies jostle for their place in this complex market - I think that one of the differentiators will be the types of end effectors they release, the strategy of disposability, and the strategy around how they commercialise the instruments. But I feel strongly that in the middle of a procedure it is the red square in front of the surgeon and the way the instrument interacts with the tissue that is still one of the most important things.






Excellent content, thank you!
Don't forget - as a subscriber you can suggest content for me to write on.