Who owns surgical stapling outcomes owns surgical stapling in the future
- Steve Bell

- Oct 29, 2024
- 21 min read
Updated: Jul 30, 2025

Staple line leaks are often deadly. Literature shows leak rate ranges between 1% to 5% depending on specialty, centre and surgeon. But the real number, I suspect, is way higher than that across the general population of patients, specialties and surgeons. In fact there is lots of data and clinical trials that support this. A simple review of the FDA Maude database some years ago resulted in a reclassification of surgical staplers. Why - Because the impact of a leak can be fatal, with a Clavien-Dindo grade II or higher complication attributed to stapler issues.
One of the challenges with stapler leakage is that the root cause of any individual’s leak can be varied and often multi factorial. From user technical errors to underpinning biological factors of the patient.
We also have to consider the usage of the stapler (Transection vs anastomosis) the procedure the stapler is being used in (Thoracic is very different to bariatric is very different to colorectal) plus the co morbidities of the patient, and of course the general use of good surgical technique that sets the surgeon up for good stapler use.

In the early 90’s I spent much of my time helping run stapling courses with some of legends of "good surgical technique" - and we diligently followed the principals of Halsted. “In 1887, Halsted stated the basis for a safe anastomosis: gentle handling of tissues, meticulous hemostasis, preservation of blood supply, strict aseptic technique, minimum tension on tissues, accurate tissue apposition, and obliteration of dead space.(NIH).”
Still today these sound principals hold true. Yet I see that many surgeons (seems to be more nowadays) do not adhere to all of these principals. Instead many (especially younger surgeons) seem to have a false belief that it is all in the stapler… so therefore “Fire and forget.” That can be a fatal assumption.
In my mind there has been too much attention on “automation” of the firing cycle and a loss of the “art” of stapling. In a great part I do feel this is down to a commoditisation of staplers, poor marketing messages, the withdrawal of support of stapling workshops and many great surgeons hitting retirement and so that tribal knowledge is being diluted or lost.
But as with most modern surgery - technology actually can play a part in ensuing that the “art” can be assisted by “The science”. So today I’m not going to go too deep into good surgical technique and review what anyone with Google or Chat GPT could research in ten minutes. Instead I’m going to talk emerging tech that is here, and coming, to assist surgeons in achieving better stapling in both transection and anastomosis.
I want to move the thinking away from "the stapler" in itself and propose a discussion about my concept of 360' technological support around stapling: that I believe is the future of stapling. A move from "surgical staplers" to a holistic "Stapling support architecture."
Advanced imaging to assist in stapling
One of the single most important factors in attaining viable tissue for anastomosis is ensuring adequate and optimal blood supply to the tissue edge. Historically this has been done by “feel and eyeball” - which means a skilled surgeon was able to hold and manipulate the transacted tissue edge and feel for say pulsatile flow, or warmth, or tissue texture. A very “haptic” ability that is mostly lost with laparoscopic and robotic approaches. Also, by looking at the tissue, a skilled surgeon can “eyeball” and see if the tissue is ischemic. It’s a mixture of oozing, colour (too blanched, too oozy) and a sense of “That looks viable.”
One technology that has become more and more prevalent in surgical practice is ICG (IndoCyanine Green.) or Near Infrared Imaging. This ICG molecule in conjunction with that Near Infrared excitement - “glows”. A specific camera set up can see that “glow” and even in some instances quantify that amount of glow. One of the pioneers of this quantified ICG was Vision Sense and their iridium heat map system. (many don't know this.)

Several other companies have been applying “dye” quantification to ICG to start to give numerical readings on the amount of “blood” within the tissue. It is an “okay” surrogate marker but does have some limitations such as leakage of the dye, how and when administration of the ICG is done, and the quality of the light source, imaging sensors, lens filters and algorithms in the software.
But it is certainly an advancement. Because it allows a real time, intra-operative visual assessment a surrogate of the blood supply to a tissue edge.
One of the issues is the ICG dye, and the half life, the diffusion of the dye and the inability to accurately qualify the blood supply for oxygen transport. Ultimately the blood must be bringing oxygen and nutrients to the tissues to help with the tissue healing, or prevent necrosis and tissue death. All things that cause leaks.
Step in some of the new technologies.
Laser Speckle Contrast Imaging (LSCI)
This is an optical assessment method that has been used in industry for years. But it is now gaining use in biological applications including surgery. (Actually in reality it’s been used for over 15 years!) In the most simple terms a laser is bounced onto tissue in a structured light patter, and if anything is moving (such as a red blood cell) it causes some “Blurring” of the bounced back laser in those points - and using some pretty funky mathematics and analysis algorithms, that blurring that can be translated into speed or flow. So you can see a background of “static” tissue and areas of “Flow” where blood is moving. And you can quantify that rate of flow and create some very pretty and useful colour maps.
So if I’m bouncing this laser speckle onto tissue and blood is moving under the surface - I can technically see where that blood is going (without a contrast dye such as ICG), and estimate it’s speed.
Companies at the forefront of this type of imaging are companies like ACTIV surgical. They have created a laser speckle technology and have been comparing the results to ICG - https://www.activsurgical.com/news/laser-speckle-contrast-imaging-compared-with-indocyanine-green-in-renal-perfusion-of-a-porcine-model

So far it is being used as an adjunct technology, but as the technology improves and clinical data starts to be accumulated about the use of the laser speckle in surgery it will gain clinical credence.
Now when this is combined with ICG, you can start to get the visual cue of where perfusion is, and then with the LSCI you can actually start to quantify the “amount” of blood arriving and produce a very useful colour map.
These are starting to become very useful tools in assessing the quantity of perfusion arriving at tissue edges. And this is an important factor that supports Halstead's principals.
Why this is a watershed moment - now - is that nearly all new robotic and lap towers - are starting to come with at least ICG as base product. So this technology is becoming rapidly diffused and accessible.
Oxygen to see (O2C)
However knowing if that blood arriving is well oxygenated or poorly oxygenated blood is also useful. As a surgeon will want to determine if oxygen is being transported to, and beyond, that staple line. It is not just the quantity of blood getting to tissue but the “quality” of the blood. And one factor is the amount of oxygen being brought to the wound edge, or staple line. (Oxygen starved tissue dies - necroses - and gives late leaks.)
This is where quantifying the amount of oxygen in blood flow is starting to emerge as a vital support tool in stapling.
There are commercial products today that use combinations of doppler flowmetry and tissue spectrometry to start to understand that quantification of oxygen within tissue. This is sometimes called Lightguide Spectrophotometry.
Companies are developing systems which are able to look at “well beyond the human eye” and look at the full band of light beyond what we can see (we see the spectral range) where if using different sensors, a camera can see below the visible range (Infrared range) and above the visible range (Ultraviolet range) - and then through combinations of AI - algorithms, filtering and real time compute... actual sense can be made of those images.
This is often called “Hyperspectral” imaging. This type of advance imaging holds a lot of promise in not only visualising blood supply, but also quantifying it by giving oxygen saturation and a quantification number across a map.
Companies like UK bases Hypervision Surgical (https://hypervisionsurgical.com/) are at the forefront of these emerging technologies. But the tantalising ability to be able to see blood supply in real time - and then measure the quality of that blood supply could open up some capabilities to improve staple line outcomes. And importantly - they do not rely upon injections of ICG.

Imagine; a piece of bowel is isolated by managing its blood supply (ligating vessels) - and prior to controlling that blood supply you can actually quantify that blood supply, even see the quality of it. Then seal / ligate the blood vessels and immediately see the impact on perfusion in real time and see to what point of the bowel blood is still arriving (through collaterals etc.) Then determine that if you staple across this part of the bowel you will get X% oxygen arriving, but if you staple across another part (further back) you get Y%.
You switch between the multimodal imaging of laser speckle, hyper spectral, and maybe even ICG - and you can now be sure of the optimal place to fire your staple line.
You fire the stapler - and then you can assess the quantity of blood and quality of it traversing the staple line.
(I'm going to go one step further. Imagine you have smarts in your imaging tower that not only gives you a measurement - but pulls on a global data base - used AI and interprests the scene and actually draws you a line on the screen that says - "Staple here." Boom.)
STOP!
What in earth do I mean here?
Much of the art of stapling and how it works has been lost over the years. So let’s do a recap.
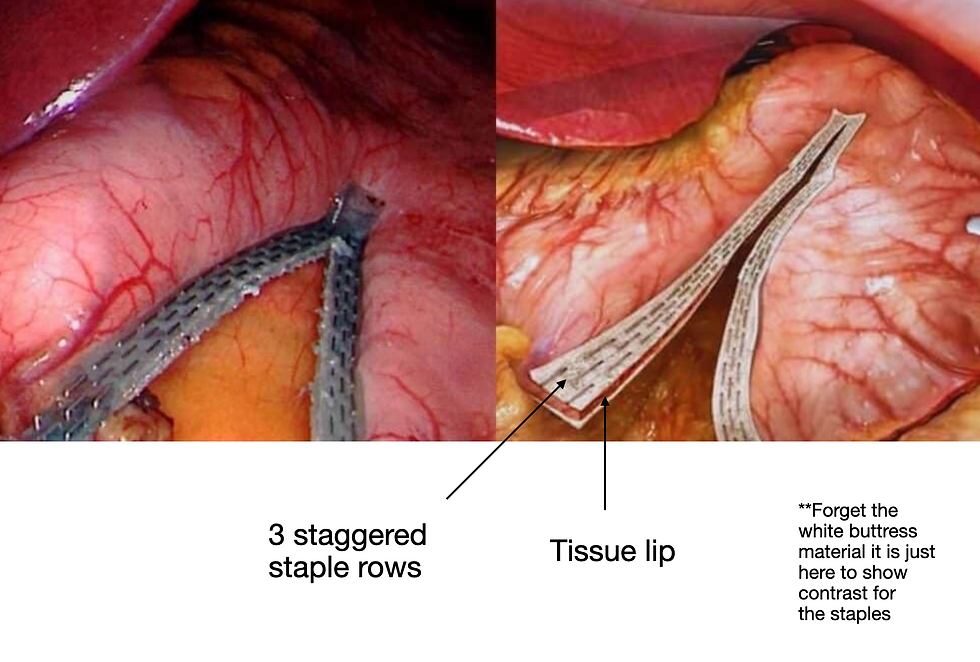
Surgical staplers push in open metal staples and they puncture the tissue - hit a metal back plate (anvil) and get bent onto a B-shape. They are not box shaped staples like a skin stapler. They are B - shaped much like you use in a paper stapler. There are just lots of them in a row. Or several staggered rows.
Why B-shaped? Well very very long history lesson to go read - but the B shape allows micro vessels to pass across the formed staple and supply blood to the very very small tissue lip this is beyond the staple line. It is this “lip” that is very susceptible to necrosis. Get the staple too tight - and you cut off the micro blood supply and the staple line and lip dies... and you get a leak.
Don’t compress it enough and the staple line bleeds too much, or tissue is not held firmly enough and bowel fluid can pass between the approximated tissue layers and —- leak.
Air can leak, fluid can leak.

Tissue compression - and optimal tissue compression is needed to get that “Goldilocks” compression that has enough oxygen supplying blood to the tissue edge post staple. But not too much that it bleeds or leaks.
Too tight = necrosis and bad.
Too loose = bleeding, fluid leaks, air leaks and bad.
That should help explain now why there are so many different colour stapling cartridges for linear Cutters - see my older stapling blog post to explain about that here : https://www.howtostartupinmedtech.com/post/surgical-stapling-in-surgical-robotics-the-next-frontier
And why when you do a circular anastomosis (end to end let’s say) you need to dial in the closure of the staple to match the combined tissue thickness. E.g. thinner tissue in the oesophagus (so more compression needed) and thicker in the colon (so less compression needed.) That means that staples must have a closure range for “Controlled Tissue compression” to hit that Goldilocks closure.

Fire and forget my ass!!!
We’re back…
So after you do that alchemy of the firing of the stapler - you can now observe with these advanced imaging modalities to asses the quality of perfusion to the staple lines, and beyond the staple lines to the lip. If that advanced imaging shows poor perfusion - then take action. Cut back tissue - use less tissue / staple compression (wind the circular less, or use a thicker cartridge.)
Why?
Now we start to get to the nub of this - if you can have a quality control pre firing - and post firing you can determine the risk that the staple line will potentially fail. And that means you can determine if remedial action needs to be performed. If you need to oversew? Add a buttress material? Remove the whole staple line and fire again?
It allows objective optionality for the surgeon. It also opens up a massive ability to qualify and quantify staple lines - pre - peri - post firing. And that is where some smart asses with AI will be able to really guide the surgeons pre and post firing - “Better to staple here doc” - “Oh that’s a shitty line - do it again.” - Asensus and Luna are already heading that way.

Intelligent imaging with AI, guidance, all based on seeing beyond the human eye is where the future of stapling lies. It is not just going to be the stapler.
Hmmm 10,000 X compute power in a DV5? Staplers in DV5? Advanced Imaging in DV5? Surgeon guidance from DV5?
Hmmmm me wonders.
But, whoever owns this advanced imaging will be able to apply a new quality control to their staplers - and that means they should get better outcomes with THEIR staplers (because of the surrounding support and data associated to their staplers, and AI based on THEIR staplers.) So they win the stapler market. You getting it yet?
Next generation surgical staplers
Okay - so now we have better assessment of the tissue before we fire - we can see where it is optimal to fire. But how about we improve the actual staplers?
Well we are already seeing this evolution of stapling technology as we start to get “Smart” staplers by Ethicon, Medtronic, and Intuitive. Better anvil designs, better firing cycles, better staple geometry etc etc.
What I mean is that (in basic terms) if you clamp down on tissue it is rarely even across the whole jaw length. There’s some bunching - there’s oedema - there’s a whole bunch of things that determine the quantity and quality of the tissue you clamp in say... an endo cutter.
In the very old days a surgeon would just pump the manual trigger and drive the staples at one speed, with a blade following behind transecting. Irrespective of the tissue thickness or resistance.
Engineers and surgeons understood that maybe at different parts of the firing cycle you have ticker tissue so you need to go slower at forming the staples and cutting (they could feel variable resistance throughout the firing cycle.)
Well step in electronics - motor drives and software. There is an “optimal” speed of staple formation and knife blade cutting for any thickness of tissue. Well the more advanced staplers have some smarts in them that do this for the user.

They will also tell a user - “tissue to too thick doc - we ain’t firing.” and lock out the ability to fire. In the old days a surgeon could just say "Nahh I know best" and force the handle until it inevitably broke - they blamed the stapler and raised a complaint.
Or the stapler will advise “too thin - it’s gonna bleed.”
Or “Big bunch of tissue here - or a crossed staple line - let me slow right down at this part.”
There’s lots of smarts that can help to give a better staple line, and that can be in both hand held or robotic staplers.
But the robot has one secret that hand helds do not. (Again see my prior posts on some of this - here - https://www.howtostartupinmedtech.com/post/caution-don-t-just-bolt-laparoscopic-instruments-on-a-surgical-robot
That secret is “Stability” while firing. The robot arm can remain utterly motionless while the stapler goes through its firing cycle - and that can remove variations in tissue tension, alterations in blood flow (stretching a vessel) that changes tissue fluid content etc etc.

The Sureform by Intuitive has tons of data about this sort of advantage. It also has a lot of sensing in the robot on tissue thickness, force during firing, forces on the tissue etc etc.
But all of these systems have one big flaw (be that hand held or robotic.) The operator needs to eyeball the tissue and say “I think I'll use a green thick cartridge on this one today.”
Then the sensors in the stapler do their magic when trying to close on tissue - or during the firing cycle. But it's a bit after the fact and well... not very scientific. In essence it's too late.
There are emerging companies such as RevMedica (www.revmedica.com) - that are building smarter next generation staplers that will take the guesswork out of tissue sizing and cartridge selection. I can’t go into too much details of “How” they are doing this - but they have a pretty “bloody obvious” idea that invokes in someone like me a "why the F did no one think of that before?"
(Medtronic and JNJ get your cheque books open now! Seriously if another company gets this...)
But all these innovations show clearly that stapling is still evolving and there is a lot more work still to do. And my future view is it's all building into a multi sensing / multi modality chain of imaging - staple sensors - ohhhhh and more below !!! It is bringing more science to the art.
So now imagine that a company has the advanced imaging that assesses blood flow and guides the user exactly where to place that staple line. The new smart stapler tells the user “use this cartridge in this section of tissue, along this path.” The robot holds that stapler at the perfect angle - rock steady - as it fires and goes through a personalised - tissue sensed firing cycle to make sure staple formation and transection are optimal.
The vision system then assesses the staple line post firing and tells the user how good that line is; and how well perfused it is along its entire length. (Maybe even if it is too well perfused and oozing.)
Any company owning this level of guidance and analysis will for sure get better outcomes - and that will mean more domination of the surgical stapling space.
Note: I’ve not gone deep on better staple line layouts, staple geometry, materials in staples, blade design, anvil design etc etc. I’m going to assume all companies are working on those iterative improvements. I will do a blog on that in the future.
Adding in Advanced Energy combinations
Instead, I’m going to head into the realms of a little more fantasy here - but I am guessing by my patent searches, and seeing the technology stacks come together... I can assume where this is actually going already.
In all staplers today the cutting (transection - staple line trimming) is done using a mechanical knife. A blade. It works and it is fine. But that blade offers no additional haemostasis beyond the staple line. So that means staple lines often have to be a little tighter that the surgeon may want and the patient may need. The issue is that if you back off on the tissue compression and staple closure - you could end up with a heavy oozing, or even gaps between approximated tissue. And that can lead to staple line breakdown.

That’s where advanced energy can be a useful adjunct as it creates excellent haemostats and tissue edge sealing.
Imagine loading a vessel sealer technology into a stapler that either cuts using cutting / sealing energy - or seals post blade cut to get better haemostasis of the staple line. Both will work. But different levels of technical application needed.
In the past, to pull that off, it meant you had to then have all sorts of combination devices in the OR - and hook those staplers into dedicated energy deliver systems.
Oh but wait - robots…
They have all of that technology combination just sitting on the "modern robotic" tower, right next to that stapler. And the robot arm delivers the stapler and the energy without having to really do anything special !!!! Virtually no extra hook ups... maybe one cable.
I’m predicting that we will soon be seeing combination stapling energy devices that will allow better - less aggressive staple closure - but sealed staple lines and better haemostasis. These new smart towers that are packed with technology can start to bring combination devices without having to go off and buy new generators specific to that device. And it will all be underpinned by AI controlling perosnalised algortihms for staple and energy delivery.
In a DV5 the Synchroseal technology and Sureform stapling technology - plus the compute power to manage both - are already there. It would not take a huge leap of technological faith (or cost) to release “Sureform plus” with integrated Synchroseal sealing / cut technology.
You see where I’m going when I keep saying that staplers will be the end effector on the robot - towers will be the weapon to deliver all that combined technology... all in one place. You think the Intuitive engineers are not sat thinking how they can put all this immense technology to work to give differentiation? To make the robot the most effective and attractive option?
This is not going to be a fight of “new robotic systems” in the next decade - it will be a fight of adjunct functionality as the hardware gets more and more capable. And I guarantee that much of this capability is already sitting right under the hood of that DV5. Software my friends... it is "just" software. (okay maybe a bit more... but you get my drift.)
Leak detection systems for anastomotic leaks
Okay so let’s recap.
We use the advanced imaging with ICG, LSCI, Hyperspectral, O2C technologies combined with AI to select the best transection site with optional blood flow.
The stapler tells the user the right cartridges to use.
The robot allows the user (from the console) to drive the stapler into the perfect position.
The smart stapler delivers the perfect staple line and transects using advanced energy to seal that line to perfection.
The AI driven advanced imaging inspects the staple line and says “Good, Bad, redo.”
The AI guidance says where to put the next line for that perfect geometry of the staple line shape profile (Bariatrics). With minimal staple line intersection.
But… that doesn’t guarantee we may still not have leaks. In an end to end circular anastomosis we might not be able to actually see and assess the inverted staple line (as it's inside the bowel away from the lap camera view.) Well in that case let’s revert to the age old and antique test of the “Bicycle” tire air bubble leak test.
WTF? It’s 2024 - almost 2025.

There is one component of the tower that we have neglected (thus far) when thinking about staple lines and anastamosis. That is the Insufflation component. The issue is that most people cannot see beyond their current paradigm and people want "faster horses.." They see insufflation as a CO2 delivery device to inflate the abdomen. They are being myopic.
But now people are realising - well we jam some filters on that we can also remove smoke. Oh and we can heat the gas and maybe add humidity, keep volume static. .. (See my post on insufflation) https://www.howtostartupinmedtech.com/post/intuitive-davinci-5-turning-up-the-gas-on-insufflation
Note: I do hope you can all now see what I’m doing here over these months to build this steady picture of the changing landscape of the OR…
And... we can monitor the gas flow very accurately, and frequently. Etc etc.
So now look where companies like Quaelon medical are thinking. It's a big feature step ahead. https://www.qaelonmedical.com/
I mentioned them in my insufflation post for very good reason. The gas (predominantly CO2) in the abdomen is almost in a sealed container. After my anastomosis, if gas starts leaking out of that anastomosis, then pressure will drop in a fairly specific way. You can even quantify that drop and start to be able to quantify the size of the leak. (Thinking of gas leaving through the staple line into say the bowel...)
In the opposite way... I know the concentration of CO2 in that closed abdomen and how much room air mixture is also in the abdomen. If I now test the anastomosis by pressure testing it with air inside the bowel… if the "air" concentration in the abdomen goes up, and the relative concentration of CO2 goes down; I’ve probably got a leak. Looking at pressure and gas concentrations I can start to quantify that leak - and start to understand if it I'll be clinical or not. (needs some clinical work but you see where this is going.) We have to start looking at insufflators as gas management and measurement systems as well as CO2 delivery systems. There will be other tech coming such as nebulised local anaesthesia, antibiotics, tissue factors, anti-adhesion etc etc - all delivered via insufflation (gas management) technology.
Back to our story: So, now the insufflator tells me I’ve got a leak - so what?
Boom - technology. I can deep dive into my smart stapler data and have AI give me a risk assessment of where it struggled in firing - where the tissue was maybe too much, if not a little thicker or thinner than I wanted. Where did the firing cycle struggle?
This data can start to now guide the surgeon to the area of concern of the leak. And we now go in deeper with the advanced imaging and see a tiny “over compressed spot” with poor blood supply. We can go in - and in real time fix the issue. Or a major ooze... or fluid leakage. Or even (in the near future) actually see the image of air leaking from a specific spot - where we can maybe see the actual leak in real time as a contrast map. (That technology exists today by the way in industry to see invading gas leaks and emissions.)
Real time we can look “Is blood flow better?”
Real time do a leak detection - “we got it.” And that surgeon can now know before that patient leaves the operating room that everything within their power was done to mange blood supply the best way, transect in the best place, have the best staple technology control the firing, seal that staple line edge, analyse that firing cycle, post fire look at blood flow and perfusion, leak test and have guidance to fix that leak. (all from one smart tower.)
And that will undoubtably lead to superior outcomes for the stapling (short term absolutely, longer term probably.)
And that will save lives, improve outcomes and save millions in healthcare dollars through the prevention of horrendous complications. And the company that does that will utterly and totally dominate surgical stapling for decades to come. It won't be about the stapler - it will be about the stapler at the heart of my proposed stapling support multimodal infrastructure that sits in their smart tower.
Who is best suited to own this complete chain of support for surgical stapling?
The clear front runner today is Intuitive! They have advanced imaging - they have stapling - advanced energy - and the all important Insufflation. They have massive compute power; and that is all packed into a very capable and convenient tower that can do robotic surgery and lap surgery. It is there today!
But let's not forget, you get the maximal stable stapling benefit when you move away from hand held staplers, and also open surgery: and use robotic stability, closed abdominal insufflation combined with their advanced imaging. (ie. want better stapling outcomes use a DV5!)

Now they may well need to buy in some tuck ins like the leak detection, next gen stapling. But they have 90% of the system right there today to start to implement this sort of 360' stapling strategy I'm proposing.
If they scoop up some of these technologies by deploying fractions of their $8 billion war chest - then it is utterly and totally game over for JNJ and MDT in stapling. It’s toast.
For Stryker and their 1788 - if they do not get these differentiated technologies focused on stapling - then their “standard” towers will have way less clinical value than say a DV5 “stapling smart” tower. And as da Vinci creeps into their lap space and demonstrates - “The DV5 tower in lap is very advanced and cool - but you add a robot and well… you get the maximum stapling benefit.” That will crush standard imaging towers everywhere.
In my opinion... Medtronic is playing catch up - as today they have an older Storz tower with no advanced imagining - not even ICG. Their stapler is coming. They do have one of the best advanced energy platforms in the world - Ligasure. But it’s not on the robot yet. And they are behind in insufflation. Is this an area they can catch up in? Why not? They are a dominant player in global stapling. (good stapling!)
JNJ have recently got IDE on Ottava - but they have not yet demonstrated stapling, tower power, advanced energy on their robot. They too need to defend that stapling empire. Are they thinking "staplers" and 360' stapling support systems? If not... I think they should be.
So MDT and JNJ have everything to lose in stapling. (Look again at Intuitive’s staggering Q3 2024 results folks.)
There is a massive defensive strategy for both of these companies to use their core strengths, and heritage of stapling to take a much more aggressive stance here. Scoop up some of these technologies fast, and build a stapling support fortress. Push a lot more effort into leapfrogging Intuitive in stapling on a robot - rather than just “get our lap product on a robot.” - Now is the time.
They have a small window to create a technology stack to release a super capable “stapler support” tower that defends their core business and builds on their heritage.
Likewise, Stryker could be the “catalyst” in the middle by having the most capable advanced tower on the market that enhances everyone's stapler - no matter what stapler the surgeon uses. They have a chance to create a “stapling centric power tower” that means anyone wanting to do advanced stapling needs to have an 1888 (1788 plus stapler analysis) - I made that up by the way.
Storz could easily do this - and concrete their tower technology by adding stapler centric advanced functionality. Oh and they do have a robot -- just saying. Just saying.
I’m going to say it again. The tower is one of the most important parts of the future surgical architecture in so many ways. It will be the technology hub enabler. And whoever develops that advanced stapler centric core capability of the tower will be a dominant player for the next decades in the OR. How could anyone NOT use their tower?
If it is one of the three stapling companies - they will be able to (I’m sure) claim that absolute best stapling solution (not just stapler) that has multimodal assists and analysis tools that holistically make their “stapling solution” the only one that anyone would ever trust.
Okay - shoot me for dreaming... But I think...
Who owns that solution owns those outcomes. Who owns those superior outcomes owns the future of the stapling market.
These are just opinons of the author for education purposes only. All trademarks belong to their respective owners.




Comments